Enhancing Accessibility and Availability of Primary Health Care Services
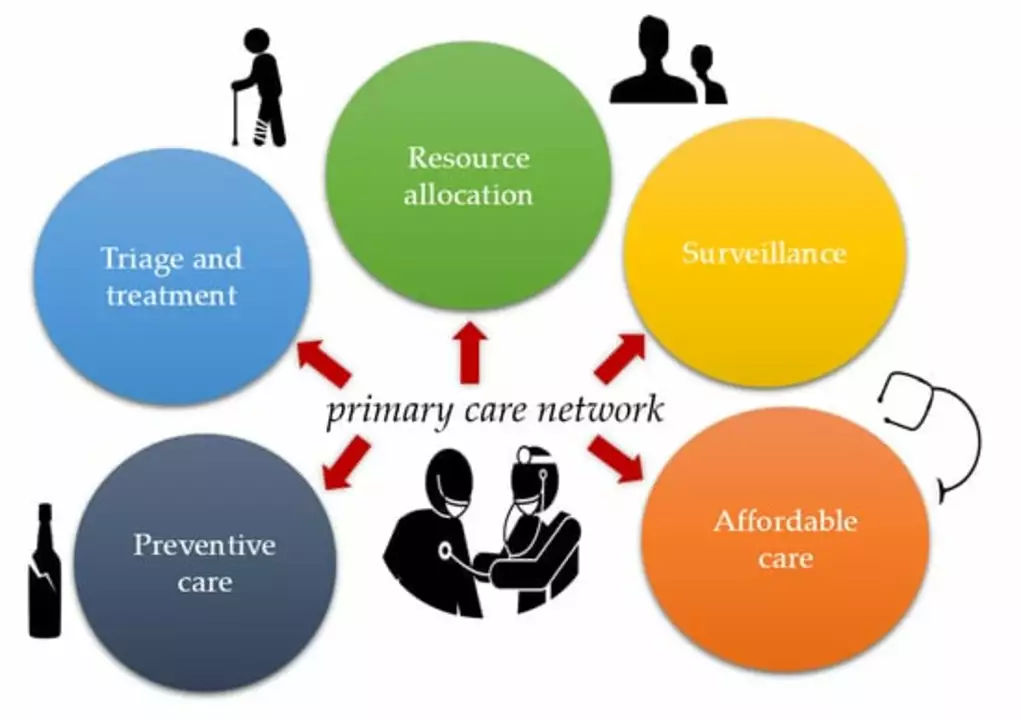
One of the critical aspects of improving primary health care is enhancing the accessibility and availability of services for all individuals, regardless of their geographical location, socio-economic status, or age. This can be achieved through increasing the number of primary health care facilities, particularly in rural and underserved areas, and ensuring that these facilities are well-equipped and staffed with qualified healthcare professionals.
Additionally, flexible clinic hours and the integration of telemedicine services can help address the needs of individuals who struggle with time constraints or limited mobility. Moreover, promoting health literacy and awareness of available primary health care services can encourage individuals to seek timely care and engage in preventive health measures. Ultimately, greater access to primary health care can lead to improved health outcomes and reduced health disparities across communities.
Strengthening the Primary Health Care Workforce
Improving primary health care also entails investing in the healthcare workforce, which includes physicians, nurses, and other healthcare professionals who provide essential services at the primary care level. Efforts to attract and retain qualified healthcare providers in primary care settings should be prioritized, such as offering competitive salaries, incentives, and opportunities for professional development.
Furthermore, training and education programs should be designed to equip healthcare professionals with the necessary skills and knowledge to deliver high-quality care and address the evolving needs of diverse patient populations. Inter-professional collaboration and teamwork should also be emphasized to ensure coordinated and comprehensive care for patients. By strengthening the primary health care workforce, we can better meet the complex health needs of individuals and communities.
Emphasizing Preventive Care and Health Promotion
Primary health care plays a vital role in promoting health and preventing diseases among individuals and communities. By emphasizing preventive care and health promotion in primary care settings, we can help individuals adopt healthier lifestyles and reduce the burden of chronic diseases. This can be achieved through regular health screenings, vaccinations, and counseling on modifiable risk factors, such as diet, physical activity, tobacco use, and alcohol consumption.
Primary health care providers should also collaborate with community-based organizations and local public health departments to develop and implement tailored health promotion programs that address the unique needs of their communities. By focusing on prevention and health promotion, we can help empower individuals to take charge of their health and contribute to a healthier society.
Integrating Technology and Digital Health Solutions
Technology and digital health solutions offer significant opportunities to improve primary health care by streamlining processes, enhancing patient-provider communication, and facilitating access to essential health information. The integration of electronic health records (EHRs) in primary care settings can help healthcare providers make informed decisions, coordinate care, and track patient outcomes over time.
Telemedicine services can also be utilized to provide remote consultations, follow-ups, and monitoring for patients with chronic conditions or limited access to in-person care. Furthermore, mobile health applications can be harnessed to support self-management of chronic conditions, promote healthy behaviors, and improve treatment adherence. By leveraging technology and digital health solutions, we can enhance the efficiency and effectiveness of primary health care delivery.
Measuring and Evaluating Primary Health Care Performance
Continuous monitoring and evaluation of primary health care performance are crucial for identifying areas of improvement and ensuring the provision of high-quality care. Establishing standardized performance metrics and indicators can help track progress, assess the impact of interventions, and inform evidence-based decision-making at the policy and practice levels.
Regular feedback and reporting mechanisms should be in place to facilitate the sharing of best practices and lessons learned among primary health care providers, and to inform quality improvement initiatives. By measuring and evaluating primary health care performance, we can identify gaps and prioritize areas for improvement, ultimately contributing to better health outcomes and a more efficient healthcare system.